Temporomandibular Disorder (aka Temporomandibular Joint Dysfunction or TMD/TMJD) is not as terrifying, but it can be a real pain. TMD affects about 20-30% of the adult population to some degree1, is more common among younger persons aged 20-40s1, and affects more females than males2.
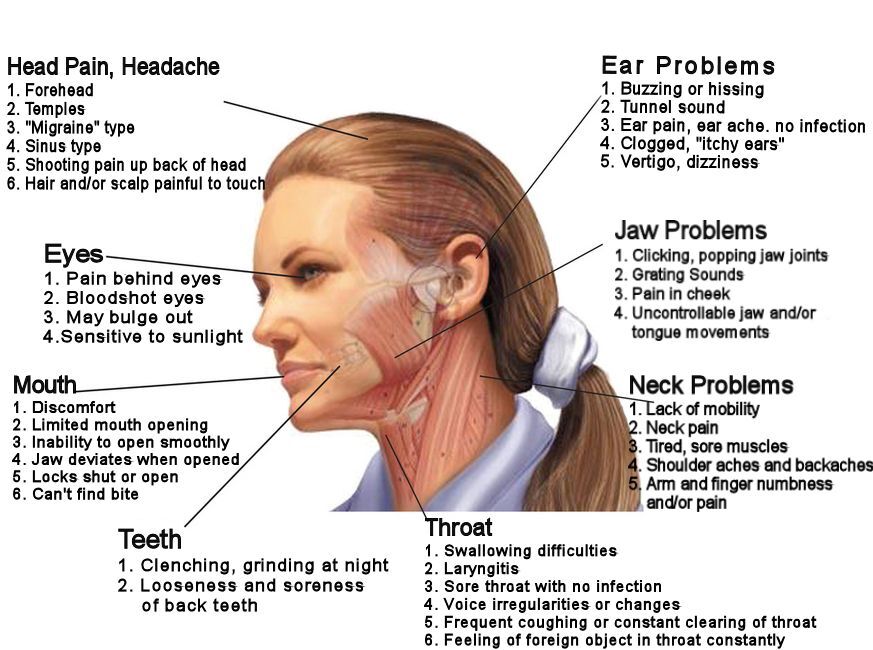
If you are experiencing one or more of the symptoms below, you may have TMD:
- Pain or stiffness in the joint and/or muscles of the jaw
- Jaw joint sounds/noise (e.g. clicking, popping or grating) when opening or closing mouth
- Difficulty opening or closing or locking of the jaw
- Difficulty chewing, swallowing or yawning
- A bite that feels “off”
- Bruxism or grinding of teeth
- Sensitive teeth
- Burning, shooting, electric shock-like facial or mouth pain
- Numbness or tingling around the jaw
- Pain or soreness in front of the ear, cheek, temples or behind the eyes
- Ear pain/ache, pressure, fullness, ringing in the ears (Tinnitus)
- Pain in the neck and shoulders
- Chronic headaches and tiredness
- Dizziness
The TMJ is formed by the temporal bone of the skull connecting to the mandible (lower jaw) and its condyle on each side of the face just in front of the ear. They open and close like a hinge and they slide forward, backward, and side to side. As with other joints in the body, the bony surfaces of the TMJ is covered with cartilage. Plus, like the knee joint, the TMJ surfaces are separated by a small disc (meniscus) that cushions the bones from rubbing against each other and helps to stabilize the joint. The muscles that open and close the mouth also serve to stabilize the joint.
Causes of Pain
TMD is a complex disorder where there can be one or multiple causes and, at times, no obvious cause can be found. Some known causes are the following:
- Trauma – can be direct (fracture of the mandible, overuse or over-opening of the mouth) or indirect (physical accidents, dental work or poor dental habits)
- Parafunctional activities/habits – teeth or muscular clenching, grinding (bruxism), stress or teeth occlusal dysharmony, excessive gum chewing or forceful biting on hard foods
- Growth plate disorders
- Posture – improper sustained spinal posture such as forward head posture or resting phone on shoulder
- Primary cranial dysfunction – abnormal development of mandibular condyle bone or tissue (neoplasm) which may or may not be pathologic
- Inflammatory conditions – infectious or traumatic arthritis, metabolic (gout) or degenerative joint disease, ankylosing spondylitis, rheumatoid arthritis (adult or juvenile) or psoriatic arthritis
- Dentition or Malocclusion – loss of teeth especially posterior teeth, cross-bite or over-bite, osteochondritis (cartilage or bone in the joint is inflamed), premature occlusal contact, prolonged procedures, braces or appliances
- Iatrogenic (inadvertent effects of procedures) – jaw wiring, multiple surgeries or ventilation, prolonged mouth opening during procedures
- Improper breathing pattern
- Psychosocial factors – such as anxiety or depression
Diagnosis and Treatment of TMD
Assessment can be performed by your doctor, dentist or physiotherapist with specialized training in TMD, and they often work cooperatively to treat the disorder. Diagnosis is best obtained using patient medical history and description of symptoms, a physical observation and examination of the jaw, neck, posture, facial structure, cranium and teeth alignment. At times, x-rays may be taken to identify any fractures or bony changes, blood tests may be recommended to rule out possible medical conditions as a cause of the problem, or MRI may be done if symptoms do not improve or worsen after a course of treatment.
Treatment of TMD may include one or more of these approaches:
- Manual physiotherapy of the joints and soft tissue of the TMJ, cervical to thoracic spine and cranium, self-acupressure
- Therapeutic exercise to address muscle imbalances and to promote proper posture and breathing patterns, relaxation and aerobic exercise
- Behaviour modification such as eating soft foods and avoiding extreme jaw movements (i.e., wide yawning, loud singing, and gum chewing)
- Modalities such as acupuncture, ultrasound, laser, applying ice or moist heat, electrotherapy and biofeedback
- Stress management, relaxation and cognitive-behavioural therapy
- Orthodontic appliance therapy such as occlusal splints, night guards and braces
- Medication such as NSAIDS, acetaminophen, muscle relaxants, antidepressants, steroid injection
- Surgery, if conservative treatment is unsuccessful
References
- Guo C, Shi Z, Revington P (2009). “Arthrocentesis and lavage for treating temporomandibular joint disorders”. The Cochrane Database of Systematic Reviews (4): CD004973.
- Edwab RR, ed. (2003). Essential dental handbook : clinical and practice management advice from the experts. Tulsa, OK: PennWell. pp. 251–309.
Information prepared by Jerrick Yao, Registered Physiotherapist
At Motion Fit Rehab and Wellness, our therapists have specialized training and experience in the assessment and treatment of TMD. If you or someone you know are experiencing any of the symptoms above or if you have any questions, please don’t hesitate to contact us.